Suffice it to say that it is an understatement that Covid-19 has altered the healthcare landscape. Despite the obvious disruptions, there have been several underlying disruptions to the US payer market from the reduction of screenings, elective procedures, or face to face meetings. Medical Marketing Economics (MME), LLC, an Indegene company explored in greater detail how the pandemic affected US payers in their day-to-day business and their interactions with biopharmaceutical manufacturers.
We surveyed 35 payer decision makers in the US to understand the impact of Covid-19 on their operations and published the findings in a new white paper, ‘Covid-19 disrupted payer operations’. The survey respondents accounted for over 165 million covered lives, and were a mix of medical directors and pharmacy directors. The paper is available for direct download without the need to share personal details at https://www.indegene.com/insights/article/covid-19-disrupted-payer-operations
While the market was disrupted, payers’ operations were exacerbated by issues such as delayed elective procedures, increase in Covid-related hospitalization, and managing a remote workforce, two key themes arose from examining payers’ data. The first, payers have expanded access to providers for conducting and receiving reimbursement for virtual visits and home care. Second, payers reduced their face-to-face interactions with biopharmaceutical manufacturer representatives but look to resume those activities in the future.
For telehealth, payers were initially unprepared to support adjudication of claims for virtual visits, but in the pandemic, this increased reliance on telehealth was rated as the top disruptor as many payers were not equipped to adapt to it. Ultimately, telehealth has become a key component of payer activity in the time of Covid-19, with 30% of payers saying that they had implemented more telehealth options and 100% confirming they would reimburse telehealth moving forward.
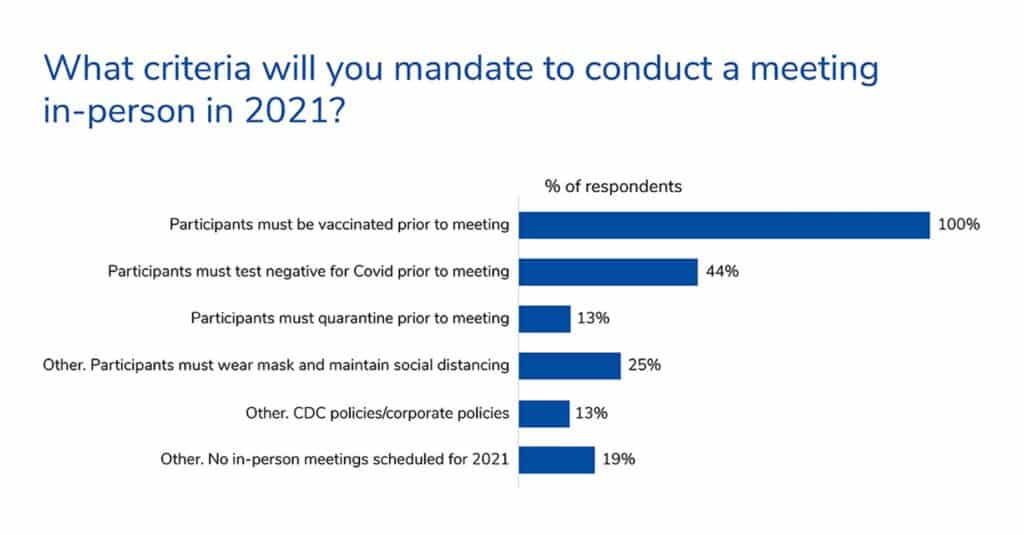
For payer-manufacturer interactions, 2020 and likely the delta variant reduced the face-to-face interactions. Payers were happy with the speed with which biopharmaceutical manufacturers adapted to video calls to replace face to face meetings. For 2021, 20% of payers had not resumed face to face meetings, but over a third of payers anticipated resumption of face-to-face meetings in 2022. However, for a face-to-face meeting to occur, payers expected representatives to be vaccinated and have a negative Covid test.
In the future, if a manufacturer has a therapy that can be supported through telehealth visits or follow-ups, it may be possible for physicians to engage with patients virtually and be compensated for that activity. Manufacturers should consider how to support providers with digital assessment materials where appropriate.
When it comes to interacting with payers, planning for a digital-first solution to communicating with payers by account managers and medical science liaisons will be critical at least through 2022.
For more such in-depth insights and 10 insightful charts on the financial, operational and network impact across a range of therapy areas, download the paper now.





